CASE # 1
A 30 years old male was brought to the hospital emergency department with presenting claim of high grade fever, stiff neck and vomiting episodes for last couple of days. On examination, the physician suspected of Meningitis. Blood samples & C.S.F samples were drawn & sent to laboratory which confirm the presence of meningitis.
1. What physical tests should be performed to confirm meningitis?
2. What empirical therapy in this condition is recommended?
3. After confirmation, what definitive therapy should be started?
4. Give picture of C.S.F., dose, dosing interval, duration of dosing and pharmacist interventions.
5. Mention some of the drug interaction in the regimen.
1. PHYSICAL TESTS FOR MENINGITIS:
A family physician or a pediatrician can carry out a physical examination, some diagnostic tests and study the medical history to diagnose meningitis. Physical examination includes checking for “…signs of infection around the head, ears, throat and the skin along the spine.” Diagnostic tests include:
Throat Culture: A throat culture can identify the bacterium that causes throat pain, neck pain and headache in the patients but would not be helpful in identifying the pathogenic microorganisms in the spinal fluid.
Radiological Studies: Imaging techniques such as X-rays and Computerized tomography (CT) scans of chest, skull and sinuses can reveal inflammation and help the doctor detect infections associated with meningitis.
2. EMPIRICAL THERAPY FOR MENINGITIS:
Antibiotic treatment of meningitis
Treatment before hospitalisation*
Benzylpenicillin (60 mg/kg, up to) 3 g intravenously or intramuscularly
or ceftriaxone (50 mg/kg, up to) 2 g intravenously (in patients hypersensitive to penicillin or in remote areas where further parenteral therapy may be substantially delayed [over 6 h]).
Empirical treatment in hospital
Cefotaxime (child, 50 mg/kg up to) 2 g intravenously, 6-hourly
or ceftriaxone (child, 100 mg/kg up to) 4 g intravenously, daily in 1 or 2 divided doses for 7 to 10 days
plus benzylpenicillin (child, 60 mg/kg up to) 1.8 g intravenously 4-hourly for 7 to 10 days (if aged under 3 months or over 50 years).
Vancomycin (15 mg/kg up to) 500 mg four times daily intravenously or rifampicin (20 mg/kg up to) 600 mg daily should be added if Streptococcus pneumoniae is suspected on Gram stain, to ensure adequate cover for penicillin- or cephalosporin-intermediate or -resistant isolates before susceptibility results are available.
3. DEFINITIVE THERAPY FOR MENINGITIS:
Specific treament (organism and susceptibility known)
Haemophilus influenzae type b
Cefotaxime (child, 50 mg/kg up to) 2 g intravenously 6-hourly
or ceftriaxone (child, 100 mg/kg up to) 4 g intravenously daily in 1 or 2 divided doses for 7 to 10 days
or, if the organism is proven to be susceptible, (amoxy)ampicillin (child: 50 mg/kg up to) 2 g intravenously, 4-hourly for 7 to 10 days.
Neisseria meningitides
Benzylpenicillin (child: 60 mg/kg up to) 1.8 g intravenously, 4-hourly for 5 to 7 days.
For patients hypersensitive to penicillin (excluding immediate hypersensitivity), cefotaxime (child: 50 mg/kg up to) 2 g intravenously, 6-hourly or ceftriaxone (child: 100 mg/kg up to) 4 g intravenously daily in 1 or 2 divided doses for 5 to 7 days.
Streptococcus pneumoniae
For strains with minimum inhibitory concentration (MIC) > 0.125 mg/L, vancomycin or rifampicin plus either cefotaxime or ceftriaxone.
For penicillin-susceptible strains (MIC < 0.125 mg/L), benzylpenicillin (child: 60 mg/kg up to) 1.8 g intravenously 4-hourly for at least 10 days.
Listeria monocytogenes
Penicillin and (amoxy)ampicillin appear equally efficacious. In patients hypersensitive to penicillin, trimethoprim–sulfamethoxazole may be used alone.
Trimethoprim–sulfamethoxazole (child: 5/25 mg/kg up to) 160/800 mg intravenously 6-hourly
plus either benzylpenicillin (child: 60 mg/kg up to) 1.8 g intravenously, 4-hourly
or (amoxy)ampicillin (child: 50 mg/kg up to) 2 g intravenously 4-hourly.
• Blood should be collected for culture before antibiotic administration if facilities allow
Chemoprophylaxis for meningitis contacts
Prophylaxis is required for the index case and for all household and close contacts of patients with Haemophilus influenzae and Neisseria meningitidis infection. If in doubt, advice should be sought from public health authorities.
Haemophilus influenzae
Rifampicin (neonate < 1 month, 10 mg/kg; child, 20 mg/kg up to) 600 mg orally, daily for 4 days.
Alternatively, although data are limited, if rifampicin is considered unsuitable, use ceftriaxone (child: 50 mg/kg up to) 1 g intramuscularly, daily for 2 days.
Unvaccinated contacts aged under 5 years should be vaccinated as soon as possible.
Neisseria meningitides
Rifampicin (neonate < 1 month, 5 mg/kg; child, 10 mg/kg up to) 600 mg orally, 12-hourly for 2 days.
If rifampicin is considered unsuitable, use ceftriaxone 250 mg (child, 125 mg) intramuscularly or ciprofloxacin 500 mg orally, as a single dose.
Non-pregnant adults: Ciprofloxacin 500 mg as a single dose.
4. PICTURE OF C.S.F., DOSE, DOSING INTERVAL, PHARMACIST INTERVENTION.
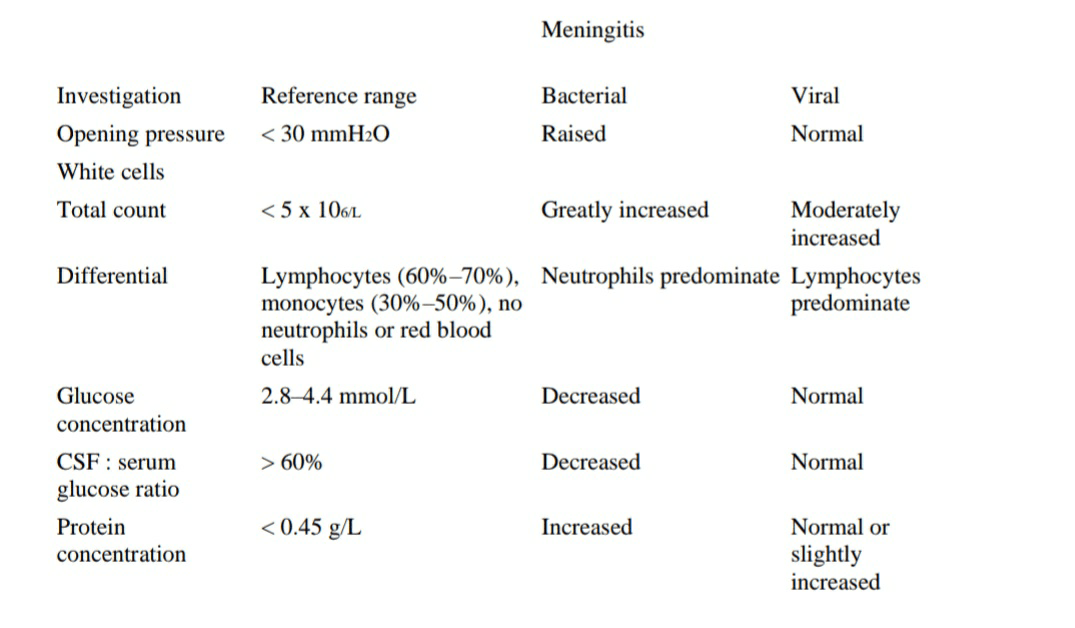
Typical profiles of cerebrospinal fluid in acute meningitis and encephalitis
INTERACTIONS:
• In empirical therapy, there is no possible interaction documented.
• In definitive therapy and in overall therapy, possible interactions may be synergism due to multiple antibiotic therapy. But in the therapeutic doses, no interaction is significant.
IMPORTANT ISSUES:
Complications:
The neurologic complications of bacterial meningitis include:
Impaired mental status
Increased intracranial pressure and cerebral edema
Seizures
Focal neurologic deficits (eg, cranial nerve palsy, hemiparesis)
Cerebrovascular abnormalities
Sensorineural hearing loss
Intellectual impairment
These complications may be sudden or gradual in onset and can appear at any time after the onset of symptoms, including after the completion of therapy. Although many neurologic complications are severe, others, such as hearing loss, may be subtle or inapparent during the early phases of infection. Early intravenous administration of glucocorticoids (usually dexamethasone) has been evaluated as adjuvant therapy in an attempt to diminish the rate of hearing loss and other neurologic complications as well as mortality in selected patients with bacterial meningitis. Hearing loss is temporally associated with the severe inflammatory changes induced by bacterial meningitis [2] and that dexamethasone reduces CSF synthesis of cytokines (such as tumor necrosis factor-alpha and interleukin-1), CSF inflammation, and cerebral edema